Glaucoma Surgery
Trabeculectomy
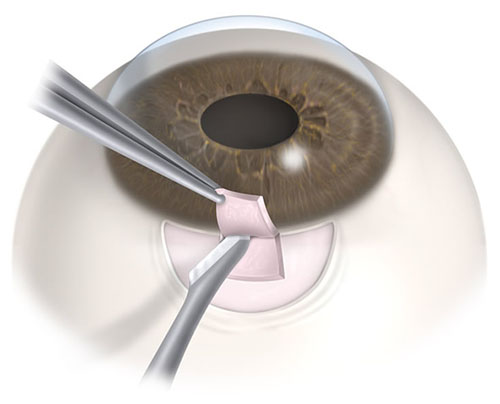
A trabeculectomy is a surgical procedure to lower the pressure in the eye to treat glaucoma. This procedure creates a new drainage pathway in the eye, which serves to bypass the blocked natural drainage tube. The benefits of a trabeculectomy are improved pressure control, a likelihood of stopping the vast majority of the eye-drops, and slowing glaucoma optic nerve damage.
A trabeculectomy is usually done under local anesthesia with intravenous sedation. The intravenous medication is used to relax the patient and reduce any discomfort associated with the procedure.
It is important to remember the goal of the surgery is to lower the eye pressure. It will not improve or restore vision previously lost from glaucoma or any other sources. In the trabeculectomy procedure, the surgeon makes a hole in the front part of the eye, which allows fluid from inside the eye to drain into the thin skin of the eye, or conjunctiva. This creates a reservoir for fluid, or “bleb.” The fluid is then taken away from the eye by the small blood vessels.
The main difficulty with trabeculectomy surgery is the variable healing response of the eye. The body will attempt to close any hole created surgically. A strong-healing patient can create too much scar tissue which seals the new hole created. The pressure in the eye can rise again, and it would be necessary to return to eye-drops or revise the surgery. If the hole totally scars down and the new drain completely fails to work, then the patient is back where they started. For this reason, anti-scarring medicines are used during the operation and afterward to slow the healing process and prevent scarring around the surgically created hole.
As with any surgery, there are risks. Risks include bleeding, infection, inflammation, eye pressure too high or too low, irreversible loss of vision, and the need for additional surgery or procedures.
The two main risks related to trabeculectomy and most eye surgeries are infection and bleeding. Infection is avoided by antibiotic drop use, and maintaining a sterile field while operating. Subsequently, there is an increased risk of infection over the patient’s lifetime. As such, if the eye ever becomes red, it is important to have the eye doctor look at it to ensure it is not an infection. Bleeding risk is typically reduced by stopping all blood thinners at least a week prior to surgery; this will be discussed with you before your surgery, and the discontinuation of blood thinners will be discussed with your medical doctor if necessary.
After the surgery, frequent visits are required to ensure the surgery is working well and to look for any early signs of failure. Patients are started on frequent eye drops to ensure the healing process happens in a predictable manner. These drops are extremely important in healing and postoperative care of the eye can make a great deal of difference in the success of the procedure.
NEVER STOP POSTOPERATIVE DROPS WITHOUT CONSULTING THE OFFICE.
The results of trabeculectomy surgery vary greatly depending on the body’s healing response. However, with care and communication with your eye doctor, there is a very good chance that your trabeculectomy will work.
Aqueous Shunts/Glaucoma Drainage Devices
Another glaucoma surgery that can lower eye pressure is implanting a tube shunt device in the eye. The goal of placing a tube shunt is to ensure the opening for fluid to exit the eye does not scar closed. Placement of this tube shunt device will not improve vision or restore vision lost from previous glaucoma damage or other sources of damage.
The implant contains a tiny silicone tube that creates a channel from inside the eye to outside and drains to a reservoir plate placed on the outside surface of the eye underneath the skin of the eye. The plate prevents the skin of the eye from sealing the tube opening. The fluid from inside the eye drains through the tube to the top of the plate and then is absorbed into the small vessels on the outside surface of the eye and into the systemic bloodstream.
The tube is covered by a piece of donor graft material which is typically preserved and specially treated. Because of the way the graft material is selected and treated, it is extremely unlikely to acquire an infection from the donor and risk of graft rejection is also unlikely.
As with any surgical procedure, there are always risks. Recent studies that compared trabeculectomy surgery to tube shunt surgery showed a lower complication rate and risk for tube shunt surgery. Some of the most common risks with tube shunt surgery are bleeding, infection, inflammation, loss of vision, need for additional surgery if the shunt becomes exposed or erodes through the skin of the eye, or eye pressure too high or too low requiring additional medication or surgery. Double vision is also a risk and may require additional surgery or removal of the implant.
There are several types of tube shunt devices available, each with their advantages and disadvantages. The most common include the Baerveldt and the Ahmed tubes. The Baerveldt takes time to heal before it starts working (typically six weeks) but achieves a lower eye pressure, while the Ahmed tube works right away after the surgery but doesn’t achieve as low an eye pressure. Your eye doctor will discuss with you which tube is best suited for your eye.
Approximately 75% to 80% of the procedures are successful, and a good portion of these patients need far fewer pressure-lowering drops. Should the glaucoma implant not adequately lower the pressure, a second implant or even sometimes a third implant can be placed if necessary.
Endocyclophotocoagulation (ECP)
Another option for glaucoma surgery is endocyclophotocoagulation (ECP), which is a laser that targets the fluid production centers of the eye. The procedure can cause inflammation in the eye. Medications can also be used along with this laser in an effort to control the pressure. There is a rare risk that the eye will not make enough fluid after the laser, causing the eye to collapse on itself or deflate. This is not painful; however, the vision can severely drop and is irreversible.
Minimally Invasive Glaucoma Surgery (MIGS)
A new generation of glaucoma surgeries has recently come to the forefront to treat mild to moderate cases of glaucoma for patients whose glaucoma is stable and who desire to reduce their need for medical treatment. This class of surgeries is generally referred to as Minimally Invasive Glaucoma Surgery (MIGS) and target the drainage tube of the eye to increase its efficiency and increase outflow of fluid from the eye to decrease the eye pressure. One of their advantages is that they can be combined with cataract surgery, thus reducing the need for multiple surgeries.
Several of these MIGS procedures involve placing a small medical device into the eye to help achieve a lower eye pressure. These devices are very small and usually cannot be seen without a microscope or special lens.
One example of a MIGS device that is currently a popular option is the iStent®. It is a small snorkel that is inserted into the drainage tube of the eye to decrease the resistance to fluid outflow, thus reducing pressure in the eye.
Some of the risks involved with MIGS procedures are bleeding, infection, inability to place the device in the eye due to abnormal eye anatomy, potential dislocation of the device in the eye, and the potential for inadequate control of the eye pressure requiring additional medications or surgery. Your eye doctor will discuss with you if a MIGS procedure could be beneficial for you.
Complications Associated With Glaucoma Surgeries
While some of the risks and complications were discussed earlier, this section will elaborate on some of the more serious risks. Infection is a severe complication associated with glaucoma surgery; this is minimized by the use of antibiotics perioperatively, and maintaining a sterile field during surgery. For trabeculectomy surgery, there is an increased lifetime risk for serious eye infections. The signs of an infection after glaucoma surgery are redness, pain, or a change in vision; should you get any of these after glaucoma surgery, you are advised to call the office immediately to notify your eye doctor. If unable to reach the office, you are to go to the nearest Emergency Room immediately and make sure to inform them you had glaucoma eye surgery.
The risk of bleeding will be decreased by the cessation of blood thinners before surgery in consultation with your medical doctor. If the pressure is excessively low during or after surgery, there is still some risk of bleeding in the back of the eye. There is also a risk of bleeding when injecting the local anesthetic. This can lead to compression of the optic nerve causing irreversible vision loss. Every attempt will be made to avoid excessive bleeding and reduce your risk.
Inflammation can occur after any glaucoma surgery. Anti-inflammatory medicines are used to prevent and treat this. The inflammation can lead to scarring which may cause your surgery to fail. Especially with trabeculectomy surgery, the need to delay healing is important to ensure the success of the surgery. After the surgery you will be on anti-inflammatory drops and your eye doctor may also supplement them with anti-scarring medication injections in the office if the surgery is healing too quickly. Regular follow-up is needed to help evaluate the healing response and ensure a successful outcome. The risk of postoperative inflammation is increased after ECP and may require aggressive anti-inflammatory control.
Decreased vision. It is important to understand glaucoma surgery cannot restore any vision already lost in the past. The goal of glaucoma surgery is to protect the remaining vision, but there is a risk of losing some or all of your vision with the surgical intervention. Every effort will be taken to minimize your risk for vision loss. Those with very advanced glaucoma may be at increased risk for vision loss because the eye is very sensitive to pressure changes.
Cataract formation may also occur. Performing glaucoma surgery can cause the lens in the eye to become more cloudy and thus cataract surgery may be necessary, sooner rather than later based on your visual needs. If you have already had previous cataract surgery, there is no risk of further cataract formation as the cataract has already been removed.
Cornea damage is possible in glaucoma surgery. There is an increased risk in glaucoma tube surgery, as the tube is placed close to the cornea. If this damage is limited, no further treatment may be needed. However, if there is contact of the tube with the cornea or if continuous flow is irritating the cornea, the cornea itself can become cloudy and a corneal transplant could be necessary. Should these signs occur, the tube may need to be re-positioned with additional surgery.
Skin of the eye over the surgery site may erode or leak. In glaucoma tube surgery, the tube may erode through the skin of the eye covering the tube. Should this occur, surgical repair and recovering of the tube would be necessary. Placing the donor graft greatly reduces this risk and is always placed to protect the eye. The graft is obtained from donor tissue and there is negligible risk of acquiring an infection from the donor source. Rejection of the graft is also unlikely. In trabeculectomy surgery, the “bleb” may become too thin or form a hole and possibly start to leak. If this occurs, another surgery may be required to seal the hole in the bleb.
Vitreous prolapse can occur, in rare instances. In this case, the vitreous jelly from the back of the eye comes forward and blocks the tube or hole in the front of the eye. Should that occur, the vitreous jelly would need to be removed with an additional surgical procedure so that proper flow is restored.
