Laser-Assisted Cataract Surgery
The Eye Specialists of Mid-Florida, P.A. surgeons strives to make cataract surgery as precise and reproducible as possible to produce the best visual outcomes for our patients after surgery. With the new improvements in lasers, we believe we cannot compete with the precision of the laser in some of the manual steps during cataract surgery.

The cataract laser softens the firm center of the cataract by breaking it up into tiny cubes. This has been shown to reduce the amount of emulsification energy needed to break up and suction the cataract out of the eye by 50% to over 90%, making the surgery gentler on the eye. We have always known the more emulsification energy that is used inside the eye to break up the cataract, the more risk of haziness of the vision for a while after surgery due to swelling of the cornea. More energy is required to emulsify more advanced, firmer cataracts. Most of the time this hazy vision recovers within the first few days up to a couple of weeks. Rarely this leads to persistent swelling of the cornea requiring a corneal transplant. Astigmatism correction with the cataract laser system has been shown to be more precise than we can do manually for both lower and higher degrees of astigmatism. It also improves the safety and accuracy of the astigmatism procedure.
Unfortunately, laser-assisted cataract surgery at present cannot be done on all patients. Small pupils block the ability of the laser to do its work on the cataract. Also, scars or cloudiness in the cornea (the clear watch glass on the front of the eye in front of the pupil and the cataract) block the laser beam enough to prevent the laser from making the incisions or softening the cataract, or both.
Over the last couple of years, the laser companies have incorporated a second laser into the instrument to precisely measure and image all of the structures in the front of the eye where the cataract surgery is performed. This second optical coherence tomography (OCT) laser is very similar to the OCT laser that our eye doctors use in the clinic every day to look at the precise details in the structure of the macula and the cornea. The accuracy of measurement of the OCT laser has been improved to less than 5 microns over the last 10 years (a single red blood cell is 7 microns in thickness). The precise images of the structures in the front of the eye now allow the laser surgical systems to make the necessary incisions and perform the softening of the cataract with exquisite control.
We believe that the Eye Specialists of Mid-Florida, P.A. surgeons do excellent manual cataract surgery, and patients get good visual results with manual surgery. However, since the laser-assisted cataract surgery is more precise and gentler on the eye, which improves patient safety and enhances the visual outcomes, we now believe it is worth the extra expense and recommend the laser-assisted cataract surgery to our patients.
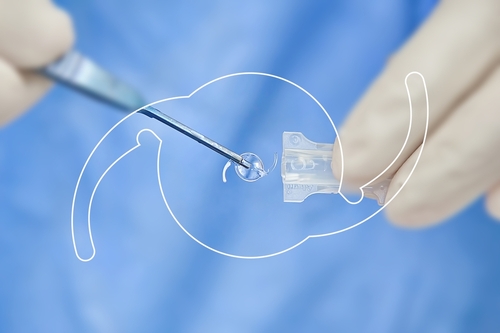
Bladeless laser-assisted cataract surgery
In 2011, the laser-assisted cataract surgery device became commercially available to surgeons. Many of the surgeons who have acquired the lasers have started advertising these as Bladeless Cataract Surgery. However, the University of Utah surgeons at Salt Lake, after using their laser system for a few months, found that they had to remove the bladeless reference in their advertising since many of the laser-created incisions were incomplete. This requires completing the incision using standard diamond or stainless steel blades.
Some surgeons are also modifying their LASIK Laser Systems to create cataract surgery incisions at the edge of the cornea and marketing it as Bladeless Cataract Surgery. These laser modifications are not FDA approved. However, they are still being marketed as Bladeless Cataract Surgery and used on patients in some areas of the U.S. We know of no university centers that are doing this, so it may be difficult to find out whether these laser incisions are frequently incomplete and require finishing with standard diamond or stainless steel blades. Also, the modified LASIK lasers do not soften the cataract to make the surgery gentler on the eye or make the precision opening in the lens capsule as the true laser-assisted cataract surgery instruments do. The additional patient out-of-pocket charge remains essentially the same per eye no matter which type of laser is used to assist in the cataract surgery.
Focusing The Lens Implant For Your Best Vision
When we are performing a patient’s first eye cataract and lens implant surgery, even if the patient wants good distance focus, we are obligated to target a minor degree of nearsightedness (-0.5 diopters) to accommodate for the known minor variability in our computer formulas for lens implant power calculations. We find it better to leave the patient with a minor degree of nearsightedness on the first eye, which is more useful for the patient than to risk overshooting beyond distance focus without glasses, which leaves the patient dependent on glasses to see both far away and up close. When we do this, we know that 90% of our patients achieve good distance vision. Due to the calculation variability, 5% to 10% of patients will achieve moderate distance vision, but also gain good vision at arm’s length and moderately improved reading vision (what we call blended vision in our custom-matched aspheric lens implant program). Also, 2% to 3% of patients achieve good reading vision but fairly hazy distance vision due to the moderate variability of the lens implant power calculations in a few eyes (we call this monovision). Many pre-cataract patients ages 50 to 60 years old will intentionally do monovision with contact lenses in order to minimize their need to wear reading glasses.
Once we determine an individual patient’s final focus on their first eye after surgery, we choose the computer formulas that best predict that final focus. We apply an adjustment factor to predict the lens implant power to use in the patient’s second eye for best distance focus without glasses if that is what the patient desires.
Doing all of this, we find that very few patients desire touch-up laser vision correction to sharpen the distance vision even on the first eye later on. The 5% to 10% of patients that inadvertently end up with either blended vision or monovision find that the closer focus in one eye greatly diminishes their need for reading glasses. Naturally, when we do not meet our complete objective of good distance vision without glasses, we, as well as some patients are initially disappointed. However, patients find by fitting them with a contact lens to correct the closer-focused eye for distance, the significant increase in the need for reading glasses is not worth the trade off. They usually elect to keep the blended vision or monovision to minimize the need for wearing glasses for casual reading. They rather elect to wear glasses as needed to drive out of town, night drive, and for prolonged reading or reading small print.
Since the computer lens implant power calculation formulas improved significantly in the 1990s, the surgeons at the Eye Specialists of Mid-Florida, P.A. have remained committed to having the very best equipment and most up-to-date computer calculation formulas available for our patients to achieve the very best vision results after cataract and lens implant surgery. The results have been very successful for our patients. We track our final vision outcomes after each surgery every one to two months on each of the three lens implant models that we use in our custom-matched aspheric lens implant programs, as well as our astigmatism (Toric) and bifocal lens implant programs.
With the recent (2014) purchase of the LenStar, the most accurate laser instrument that measures all of the parameters of the eye necessary for our lens implant computerized power calculation, we have improved the final focus accuracy to plus or minus 0.5 diopter in over 90% of our patients. We also utilize five or six of the most advanced computer formulas on each patient to help ensure this accuracy.
Since 2014, the Eye Specialists of Mid-Florida, P.A. surgeons would choose the laser-assisted custom-matched aspheric lens implants (or Toric lens implant, if appropriate) for themselves and/or their family members. In fact, this is what we have done for Dr. Welch’s father, mother, and mother-in-law over the last few years.
Short wait before second eye cataract surgery

As noted previously, there is a mild variability in our ability to predict the implant power to get excellent distance vision without glasses and 5% to 10% of people will end up mildly near-sighted on the first eye after surgery. The exact focus of the eye can vary slightly over the first week or so after surgery as the implant heals into the eye. Therefore, we like to have at least a week before the second eye surgery so we can accurately measure the final glass prescription that will be needed on the first eye to see if it’s off of a good distance focus without glasses. Having this information helps us go back to the lens implant power calculations and more accurately predict the implant to use on the second eye to be sure we get good distance vision without glasses on the second eye.
Anterior chamber intraocular lens implants
After intracapsular cataract extraction, and occasionally after extracapsular cataract surgery, an anterior chamber intraocular lens implant is performed. This lens implant is inserted in the anterior chamber of the eye between the iris and the cornea. Anterior chamber intraocular lenses can also be implanted in patients who have had cataract surgery years ago without a lens implant and now find they cannot use contact lenses or cannot adapt to cataract glasses (secondary intraocular lens implant).
Can a lens implant now be performed after previous cataract surgery?
Yes. Most patients who have had cataract surgery performed without a lens implant can now have a secondary intraocular lens implant if they cannot adjust to cataract glasses or can no longer wear a contact lens. (See above – Anterior chamber intraocular lens implants.)
Computerized lens implant power calculations
Prior to the eye surgeon performing a patient’s cataract surgery, technicians will be obtaining a few measurements to aid the surgeon in determining the power of the intraocular lens implant.
The first reading is called biometry (either by laser or A-scan ultrasound); this is done to determine the length of the eye from the front of the cornea to the back of the eye, which is called the macula (center of the retina). For this procedure, the patient will be asked to place their chin in an instrument similar to the microscope the surgeon used when examining their eyes. The patient will look toward the red instrument fixation light while the laser biometer measures the length of the eye. The second reading is called keratometry; this is done to determine the focusing power of the cornea. The third reading will be measuring the depth of the anterior chamber.
The fourth reading will be measuring the corneal diameter. All four of these measurements are utilized in the complex computer formula calculation to determine the appropriate lens implant power for the individual patient’s eye. The procedure is painlessly performed without the need to numb the eye. Less than 5% of eyes cannot be measured with the laser, in which case the A-scan ultrasound biometer will be used. For this procedure, the eye will be numbed with drops, then a small plastic cup will be placed inside the eyelids and filled with sterile water; inside the cup is an ultrasound probe.
Sound waves travel through the eye like sonar from a submarine and measure the length of the eye in hundredths of millimeters. Because the eye is numbed with drops, these measurements are painless. Nevertheless, some patients experience anxiety during the testing. If patients relax and do not squeeze the eyelids excessively, the testing can usually be completed within a couple of minutes.
Two sets of these measurements will be performed on the eye that is scheduled for surgery to ensure accuracy. The measurements are then fed into a computer containing the most up-to-date lens implant power calculation programs, wherein the measurements are compared to data from many thousands of patients who have previously undergone lens implant surgery.
From the data, a computer calculates the proper power of the lens implant to be used for the eye scheduled for surgery.
Though most patients prefer we calculate the lens implant power for best focus at distance without glasses, other patients prefer to be able to view the computer and view their watch as well as distance vision without glasses. For these patients the surgeon can focus one eye for near vision with the lens implant by making an adjustment in the lens power calculation. Then, the second eye is focused for far vision. This process is what we call blended vision. The goal for blended vision is to function 80% of the time for normal daily activities without glasses. Glasses will be necessary for reading small print and night driving. Monovision focus with a lens implant is where one eye is focused for best distance vision and the other eye is focused for close reading vision. This allows for the patients to do most activities including reading the newspaper, signing checks, and other paper work. We currently offer monovision to patients that have been successful monovision contact lens wearers.
Most monovision or blended vision patients still require glasses for activities such as viewing the computer, or reading fine print based on the patient’s choice for the outcome of their surgery. Patients frequently require glasses for night driving if blended or monovision options were chosen. Using the custom-matched aspheric (distance focus) lens implants, approximately 90% of patients feel that they see well enough to do most distance activities without glasses. Also, about 10% of patients feel that they see well enough to do all activities without glasses. Sixty-five percent (65%) of patients use glasses only for reading and 25% of patients wear glasses most of the time, although some of these see well without glasses at distance, but just prefer to wear them.
Glasses after cataract surgery
Unfortunately, even with the most up-to-date lens implant measuring instruments and lens implants, it is impossible to guarantee that patients will be able to function for all activities without glasses after cataract and lens implant surgery. This is especially concerning in patients that have always had good distance vision in both eyes without glasses. Even in these patients, especially when doing the first eye surgery, we have the 5% to 10% chance that the eye will end up mildly to moderately nearsighted which will require glasses correction for sharpest distance vision. However, as explained in the booklet, this does make it so the patient can read moderate-sized print without being as dependent on readers.
Advanced Technology Lens Implants

Insurance issues
Starting in 2005, multifocal, accommodating and custom-matched aspheric lens implants have been approved for use in the United States by the FDA. We would like to provide our patients the opportunity to choose between the single-focus lens implants and the latest in bifocal lens implant technology. Although the out-of-pocket expense is high for these new technology bifocal lens implants, the individual patient must weigh the added value of having a 40% to 80% chance of being free of glasses for most activities.
As per Medicare and commercial (private) insurance guidelines, it has been determined that patients desiring these advanced technologies multifocal, accommodating, astigmatism-correcting (toric), or custom-matched aspheric lens implant packages are to pay for the added cost. This out-of-pocket expense will not be covered by Medicare or your supplement insurance or by commercial insurance for non-Medicare patients. These charges vary depending on the lens implant package you chose. The dollar range of these out-of-pocket expenses is available from our insurance and surgery scheduling staff.
Custom-matched aspheric lens implants (Includes Astigmatism-Reducing Incisions)
The custom-matched aspheric lens implant provides the sharpest vision, especially in low light conditions, including a 45-foot advantage in identifying objects at a distance when night driving, allowing faster reaction time. Some patients may need glasses to fine tune and obtain the sharpest distance vision. Most patients require reading glasses for near vision. This package includes astigmatism-reducing incisions when indicated, which reduces up to 1.00 diopters of astigmatism.
Blended vision with custom-matched aspheric lens implants
The custom-matched aspheric lens implant with blended vision allows the eyes to focus images for a continuous range of vision. Our goal is that you can perform 80% of your normal daily activities without glasses such as seeing far away in addition to seeing moderate-sized print on your cell phone, computer, dashboard, overhead shelves and shopping. Twenty percent (20%) of the time you will require glasses. If close reading focus is desired in the near eye without glasses, you may experience reduced depth perception. This package includes astigmatism-reducing incisions when indicated, which reduces up to 1.00 diopter of astigmatism to achieve the best vision we can without glasses.
CrystaLens
The CrystaLens is a good choice for patients who want to avoid the need for glasses in distance (arm’s length away) and social activities, but do not mind wearing readers. The CrystaLens was the first accommodating lens implant to be FDA-approved. This implant changes focus from distance to arm’s length vision by some movement of the lens implant inside the eye as the eye attempts to focus for near vision. Studies show that CrystaLens can achieve 1.0 to 2.0 diopters of near focus, whereas our usual lens implants only achieve 0.5 to 1.0 diopter of near focus.
However, we know that it takes 2.5 to 3.0 diopters of near focus to read small print comfortably; therefore, the CrystaLens is probably not a good lens implant choice for a person who enjoys a lot of reading, needlework, or other handwork activities. The hinged mechanism of the CrystaLens, which helps the movement of the lens implant in the eye for near focusing, has some potential difficulties in a small number of patients. These difficulties will sometimes require repeat surgical correction (usually laser treatments). Less than 4% to 5% of patients with the CrystaLens may require removal of the lens implant (due to these problems) and have a replacement lens implant of a different type. In our standard single focus lens implant surgery, the risk of needing to remove and replace a lens implant in the early period after surgery is less than 1 in 1,000.
Multifocal lens implants
The ReSTOR, Symfony, and Tecnis multifocal lens implants have been approved by the FDA. These types of lens implants require basically the same surgery as our regular lens implants. The FDA studies on the ReSTOR, Symfony, and Tecnis multifocal lens implants showed that after both eyes were implanted, about 80% of patients were spectacle-free. These lens implants give good vision for distance and for intermediate distance reading (computer screen/arms length) range. However, low power reading magnifiers may be needed for small print.
The ReSTOR, Symfony, and Tecnis multifocal lens implants simultaneously focus both distance and near images inside the eye. Frequently, it will take some time for patients to adapt to having two images in focus inside the eye, since this seems to degrade the sharpness of the distance vision very slightly. However, most patients do not find this to be a significant problem. We know glare problems with the ReSTOR, Symfony, and Tecnis multifocal lens implants are frequent enough to always discuss them with patients before considering surgery. We only use these lens implants in patients who feel that some night glare would not be a problem. Even after these discussions and pre-selection, 20% of patients with the ReSTOR, Symfony, and Tecnis multifocal lens implants report moderate glare difficulty, especially with night driving, and 3% to 5% of patients report severe glare difficulties. Long term studies show that about 1% to 2% of patients may have such severe glare difficulties or problems with “waxy” or “fuzzy” vision that they will want the multifocal lens implant removed and replaced.
Other than problems with glare and a mild decrease in vision clarity, there is a low likelihood of having other difficulties with these lens implants that would require repeat surgery.
Many patients are willing to trade off the deficiency of some glare difficulties and a slight decrease in the sharpness of distance vision for a much greater chance of not having to rely on readers and are very happy with the ReSTOR, Symfony, and Tecnis multifocal lens implants.
