What is the Retina?

The human eye is best compared to a camera. The camera lens focuses light from an object to form an image on the film. The compound lens system of the eye (cornea and lens) similarly focuses light from an object to form an image on the retina (the layer of nerve cells in the back of the eye). The optic nerve transmits these images to the brain. The dark spot in the center of the retina is called the macula. The macula allows you to see tiny details and is responsible for your central vision. Reading fine print, recognizing faces, color vision, and being able to drive are all responsibilities of the macula. Maintaining good health of the macula, as well as the entire retina, is essential for your best vision. There are many conditions that affect the retina.
Common Retina Disorders:
Macular Degeneration (AMD)
Age-related macular degeneration (AMD) is the leading cause of vision loss in people over 55. Macular degeneration is a very common condition and affects one in five people aged 70-84. It is age-related, and by the time we are 85, almost half of us will have some degree of macular degeneration. There is a whole spectrum of disease, ranging from very mild changes to the more severe. This disease affects the part of the retina called the macula.
The retina is the nerve tissue lining the back of the eye, and it is this nerve tissue that lets us see. The macula is a small part of the retina, but it is a very important area because half of the nerve cells live there. The macula is responsible for (1) your fine, detailed vision (everything smaller than the big “E” on the eye chart), (2) your straight-ahead vision (when you look at someone’s face), and (3) your color vision. The macula is not responsible for your side vision or night vision.
So, when you have macular disease, even at its worst, you do not go completely blind. You can still see to get around and to do things for yourself, however the disease may affect your ability to read and drive. The major risk factors for macular degeneration include family history, smoking, uncontrolled hypertension (high blood pressure), high cholesterol, and obesity.
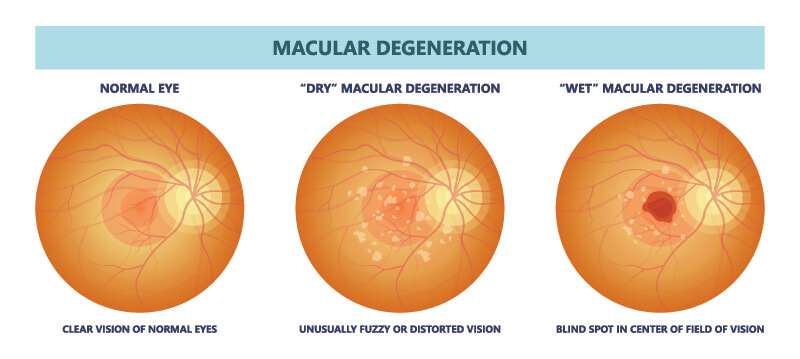
Dry (or Non-exudative) Macular Degeneration
In approximately 90% of patients, macular degeneration presents as the “dry” type. In dry macular degeneration, the retina gradually thins out (becomes atrophic), and pigmentary changes may occur, along with lumpy deposits under the retina called “drusen.” The changes are most pronounced in the macula, and there may be a slow, gradual drop in the central vision. In most people, these changes occur over a period of years to decades. The condition may affect both eyes, but is often asymmetrical, affecting one eye much more than the other.
Wet (or Exudative) Macular Degeneration
In about 10% of patients, abnormal new blood vessels grow under the retina, where they may leak fluid and bleed. When this happens, we call it the “wet” type. With wet macular degeneration, you still do not lose your side vision, however the central (reading) vision may drop rapidly, sometimes in a matter of days to weeks. If we can catch it early, we now have effective treatments that may slow or stop the progression of the disease.
Detection and Testing
In the earliest stages of macular degeneration, the vision may be normal. Over time, there may be a loss of contrast, sensitivity, faded colors, and central blurring. Checking each eye (one at a time) for distortion on the Amsler grid can catch early changes. Even before symptoms develop, it may be possible to detect macular disease with a dilated eye exam. People over 65, especially those with a family history of macular problems, should have annual eye checkups. Specialized testing can often help the doctor identify subtle changes, locate and measure leakage, and evaluate the retinal circulation. Optical Coherence Tomography (OCT) is a quick and painless scan of the eye, which shows the thickness and contour of the retina and underlying tissue. Digital Angiography gives a detailed view of the circulation and can identify hidden abnormal blood vessels.
Treatment for Dry AMD
There is no “cure” for macular degeneration, however we do know that certain nutritional supplements may slow the progression of the disease and reduce the chances that dry AMD will progress to the wet form. The Age-Related Eye Disease Study (AREDS) showed that a specific formula of Vitamins A, C, E, Zinc and copper is beneficial for non-smokers. Other supplements, such as lutein and omega-3 fatty acids (found in fish oil) may also help, along with dark green, leafy vegetables. We offer a supplement called, MacuHealth which is available at all our locations.
Treatment for Wet AMD
There are now very effective medicines for treating Wet AMD, some of which are introduced into the eye at regular intervals using a very tiny needle. If left untreated, wet macular degeneration usually results in loss of the central vision. With these new medications and timely treatment, we are now able to maintain vision in up to 90% of patients and can actually improve vision in up to 40%. Our doctors have extensive experience in the diagnosis and management of both wet and dry AMD. Regular eye exams, with prompt treatment, when necessary, offer the best hope for preserving vision. It is much easier to hold on to what you have than it is to recover what you have lost.
Diabetic Retinopathy
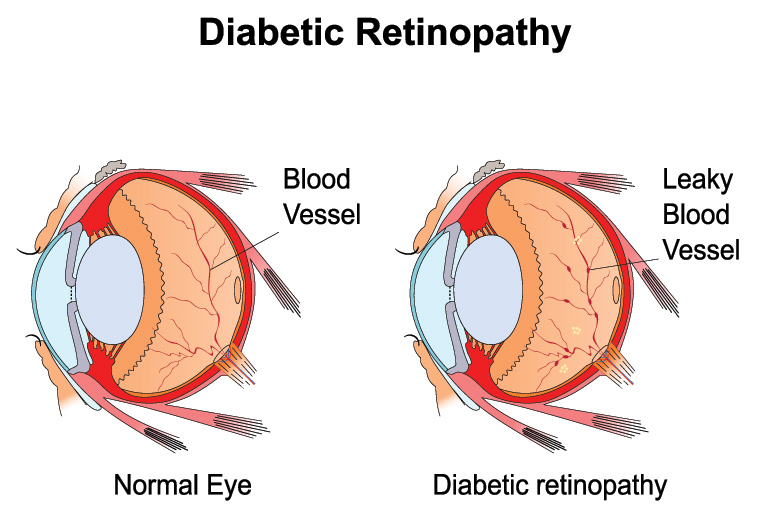
Diabetes is a disease that affects small blood vessels throughout the body. The retina is the nerve tissue lining the back of the eye, and it is this nerve tissue that lets us see. Small blood vessels run through the retina, supplying it with blood. When diabetes affects these retinal vessels, it can affect your vision. Almost everyone who has had diabetes for more than ten years will have some changes visible in the retina. People often have diabetes for a while before it is diagnosed, and the changes can sometimes show up sooner.
Diabetic Macular Edema (Retinal Swelling)
One of the things that can happen in diabetes is that the normal blood vessels in the back of the eye can become leaky, and clear fluid can collect in the retina, making it thick and swollen. Sometimes fatty material can leak from the vessels, and the retina can accumulate yellow deposits called “exudate.” If the retinal swelling or exudate gets too close to the macula, the central vision can become blurred.
If your vision is threatened by (or has been affected by) leakage, there are things the doctor can do to try to dry up the fluid and prevent further visual loss. Treatment, including laser and intravitreal medicine, may also offer hope for visual improvement.
Proliferative Diabetic Retinopathy (Poor Circulation and Bleeding)
Another way in which diabetes can affect vision is through poor circulation. If you develop poor circulation to the eye, this may affect the macula and limit your vision. When the circulation to the retina is very poor, other problems can develop. If the retina doesn’t get enough blood, it may start to release a chemical that causes new blood vessels to grow. These are not like the normal blood vessels that can become leaky with diabetes. These are abnormal new vessels, and they are often lacy and fragile, and they may break and bleed into the center of the eye. If this happens, the eye may fill with blood, and severe vision loss may occur. If abnormal vessels are detected early, or if the bleeding is not too dense, laser treatment may help shrink these abnormal vessels and make additional bleeding less likely to occur.
Detection and Testing
A lot can be discovered with a dilated eye exam, and every diabetic patient should have regular checkups to detect retinal changes as early as possible. Sometimes advanced testing can help the doctor identify subtle changes, locate, and measure leakage, and evaluate the retinal circulation. Optical Coherence Tomography (OCT) is a quick and painless scan of the eye, which shows the thickness and contour of the retina. Digital Angiography gives a detailed view of the circulation and can be used to map out areas of leakage to aid in treatment.
Treatment for Diabetic Retinopathy
Laser treatment may be helpful for reducing macular swelling. Laser may also help with proliferative diabetic retinopathy by reducing the areas where the circulation is very poor, making the “bad chemicals” go away, so that the abnormal blood vessels can shrink. There are also now very effective medicines for treating diabetic retinopathy, some of which are introduced into the eye at regular intervals using a very tiny needle. When there has been bleeding into the center of the eye (vitreous hemorrhage), it will often clear by itself, but it is essential that the eye is examined to be certain that it is safe to observe it. Other problems can cause bleeding in the eye, including retinal tears that can lead to retinal detachment, and it is very important to know what is going on. If the blood fails to clear on its own, it is possible to remove the blood with an outpatient surgical procedure called a vitrectomy. Sometimes blood will organize and form scar tissue, pulling on the retina and causing it to come away from the wall of the eye. This is called a tractional retinal detachment, and may require surgical intervention.
Monitoring and Checkups
Diabetic patients should regularly monitor vision in each eye and should seek immediate attention if changes are seen in either eye. Changes are less likely to occur when blood sugars are well controlled, but even when there has been good control, serious problems can arise. Our doctors have extensive experience in the diagnosis and management of diabetic retinopathy. Regular eye exams, with prompt treatment, when necessary, offer the best hope for preserving vision.
Retinal Holes and Tears
Vitreous detachment is a common condition that usually affects older people, especially those who are nearsighted. Only rarely does it have any serious consequences. Most of the eyeball is filled with vitreous, a gel-like substance that helps maintain its round shape. The vitreous contains millions of fine fibers that are attached to the retinal surface (the retina is the light sensing layer at the back of the eye). As we approach middle age, the vitreous slowly shrinks away from the retina, and if the fibers pull free, it becomes detached and can cause tears or holes. If you have a vitreous detachment in one eye, the other eye is also likely to have one, though it may not happen until years later.
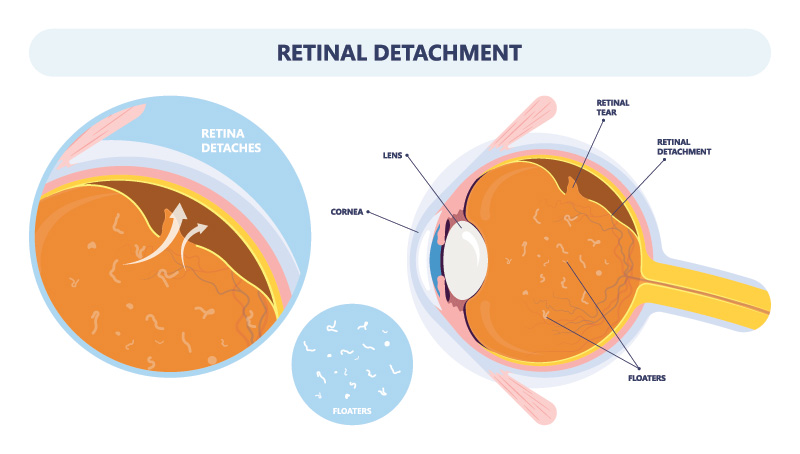
When the vitreous detaches, the number of floaters suddenly increases. Floaters are little “cobwebs” or specks that seem to float about in your field of vision; they become most apparent when you look at the sky or brightly lighted reading material. (Even if you were not aware of them, you have always had some floaters since birth.) You may also see bright flashes of light (“lightning streaks”) off to the side whenever you move your eye. These are especially noticeable when you go into a darkened room. Light flashes occur when the detached vitreous, which now moves about more freely as the eye moves, bumps lightly against the retina. Almost always, the floaters and light flashes decrease during the weeks or months after the vitreous detaches, though they may never disappear completely.
Most of the time a vitreous detachment is merely annoying because of its symptoms. However, once in a while some of the vitreous fibers pull so hard on the retina that one or more retinal tears or holes are created. These can lead to a retinal detachment – a much rarer problem that threatens vision. If a retinal tear happens to rip a retinal blood vessel, blood will spill into the vitreous and partially obstruct vision. Extensive bleeding can obscure the retina and prevent the tear or even a retinal detachment from being found during the eye exam. If you have the sudden symptoms of a vitreous detachment, your eye needs to be examined for retinal tears.
Though a vitreous detachment begins suddenly, the full detachment process can take up to several weeks. The danger of retinal tear formation continues throughout this entire period. Therefore, your retina should be examined again about 4 to 6 weeks after the initial sudden appearance of floaters. Vitreous detachment requires no treatment if there are no retinal tears. Even though the floaters and light flashes decrease with time, that does not necessarily mean that everything is all right. If a retinal tear is present, the most watery part of the vitreous might leak through the tear, causing the retina to peel (detach), like wallpaper, from the underlying layer. This is a retinal detachment.
At first, the only symptoms may be floaters and light flashes identical to those caused by the vitreous detachment. Its classic symptom appears later: a “curtain” of darkness that moves in from one direction and gradually, over a period of days, blocks out some peripheral vision. If not treated, the detachment will progress. When it reaches the central zone of the retina (the macula), it will cause sudden blurring of vision. The curtain will continue to darken more and more vision until only bright light can be seen. If, in addition, a large retinal blood vessel has been torn, blood may fill the vitreous and cause almost total loss of eyesight.
A RETINAL DETACHMENT IS AN EMERGENCY!
If you have symptoms of a retinal tear or a retinal detachment, call at once for an immediate appointment. If this is not possible, go to an emergency service or hospital. It is important for your eye to be examined by an eye surgeon as soon as possible. Early treatment can often prevent permanent loss of vision.
Macular Pucker
Macular puckers (epiretinal membranes – ERM) develop occasionally in patients, most frequently with age; and occasionally in patients with diabetes or other eye problems. Macular puckers develop from a thin layer of fibrous tissue that is laid down on the surface of the retina over a period of several months. Then, as this fibrous tissue matures, it contracts like scar tissue and puckers the retina. Fortunately, most macular puckers remain mild. Your eye doctor can see them on the surface of the retina at the time of your exam; however, they do not noticeably affect the vision. Macular puckers probably develop as the result of a process of aging of the clear jelly that fills the center of the eye (vitreous). This aging process of the vitreous also causes the floaters which many people experience with age. No one really knows why a few patients develop macular puckers as a result of this aging process while, fortunately, most do not.
Early detection is key to preserving your eyesight. Contact Eye Specialists of Mid-Florida, located in Auburndale, Clermont, Haines City, Lakeland – Harden, Lakeland – CR 540-A, Lake Wales, Sebring, and Winter Haven today to schedule an appointment.


